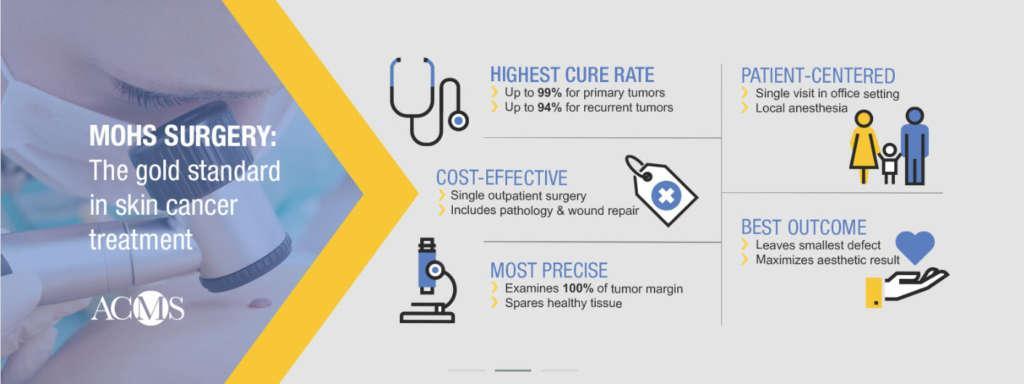
Mohs surgery is a precise surgical technique used to treat skin cancer. During Mohs surgery, thin layers of cancer-containing skin are progressively removed and examined until only cancer-free tissue remains. Mohs surgery is also known as Mohs micrographic surgery. Our highly-sought-after head surgeon, Dr. Christopher Kruse, has performed over 15,000 Mohs surgeries and reconstructive repairs.
Originally developed in the 1930s by Dr. Frederic Mohs at the University of Wisconsin, Mohs micrographic surgery has been refined into the most advanced, precise, and effective treatment for an increasing variety of skin cancer types. With the Mohs technique, physicians can precisely identify and remove an entire tumor while leaving the surrounding healthy tissue intact and unharmed. Mohs surgery offers the highest potential for cure – even if the skin cancer has been previously treated by another method.
Why choose a Fellowship-Trained Mohs Surgeon?
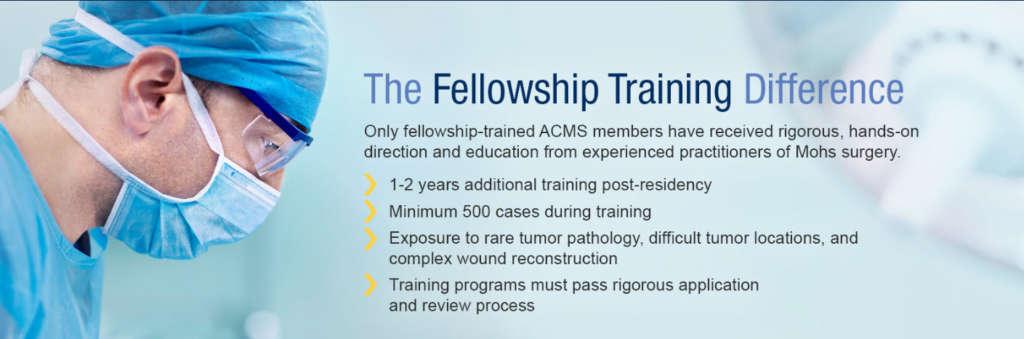
You want your skin cancer treatment to be performed with the highest standards of quality and competency. The American College of Mohs Surgery is the only organization that requires its members, after their years of residency training, to successfully complete an extensive fellowship of at least one full year of hands-on training in the Mohs procedure under the supervision of a highly qualified instructor.
Upon completion of a dermatology residency, a physician can apply to participate in a Micrographic Surgery & Dermatologic Oncology (Mohs) fellowship training program. Qualified applicants undergo an extremely competitive review and selection process to obtain a 1- to 2-year fellowship position with a program accredited by the ACMS (international programs).
Learn More About Mohs Surgery and What’s Involved
Learn More at the American College of Mohs Surgery >>